PREVIOUS
National Health Policy 2017
January 24 , 2019
2598 days
23767
0
National Health Policy
- The National Health Policy of 1983 and the National Health Policy of 2002 have served well in guiding the approach for the health sector in the Five-Year Plans.
- The health priorities are changing. Although maternal and child mortality have rapidly declined, there is growing burden on non-communicable diseases and some infectious diseases.
- The important change is the emergence of a robust health care industry estimated to be growing at double digit.
- Another change is the growing incidences of catastrophic expenditure, which are presently estimated to be one of the major contributors to poverty.
- A rising economic growth enables enhanced fiscal capacity on Health.
New Policy in 2017
- The Union Cabinet chaired by the Prime Minister in its meeting on 15.3.2017, has approved the National Health Policy, 2017 (NHP, 2017).
- It aims at achieving universal health coverage and delivering quality health care services to all at affordable cost.
Goals
- The policy is aimed at ensuring healthcare reaches all, particularly to the under-served and underprivileged.
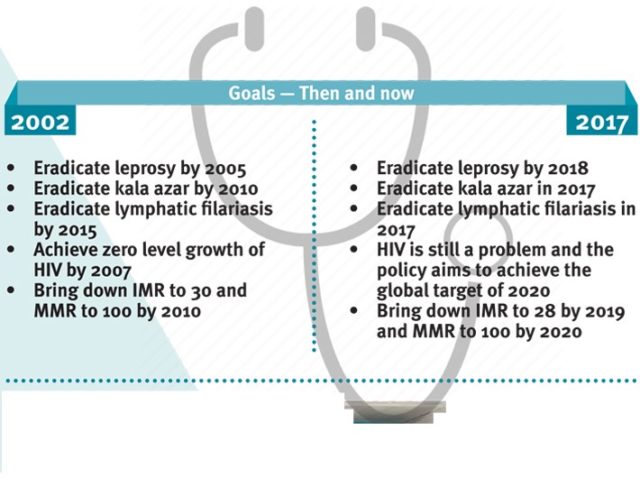
- This would be achieved through increasing access, improving quality and lowering the cost of healthcare delivery.
Objectives
- Improve health status through concerted policy action in all sectors and expand preventive, curative, palliative and rehabilitative services provided through the public health sector.
Specific Goals and Objectives
- Health Status and Programme Impact
Life Expectancy and healthy life
- Increase Life Expectancy at birth from 67.5 to 70 by 2025.
- Establish regular tracking of Disability Adjusted Life Years (DALY) Index as a measure of burden of disease and its major categories by 2022.
- Reduction of TFR to 2.1 at national and sub-national level by 2025.
Mortality by Age
- Reduce Under Five Mortality to 23 by 2025 and MMR from current levels to 100 by 2020.
- Reduce infant mortality rate to 28 by 2019.
- Reduce neo-natal mortality to 16 by 2025.
Reduction of disease prevalence/ incidence
- Achieve global target of 2020 which is also termed as target of 90:90:90, for HIV/AIDS.
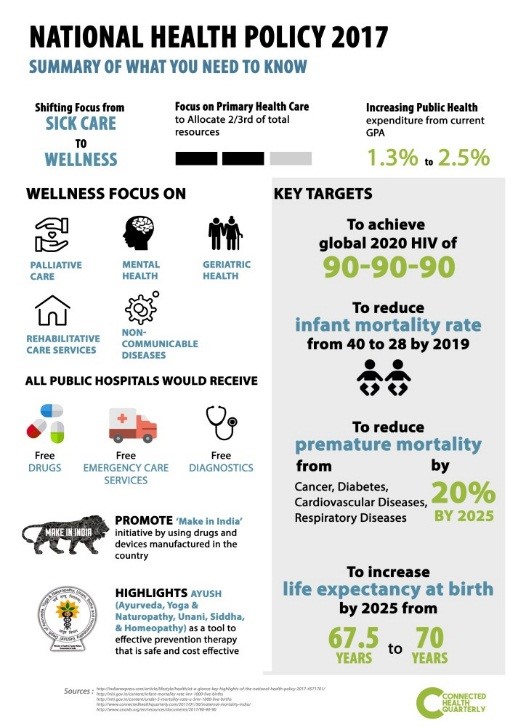
- Maintain elimination status of Leprosy by 2018, Kala-Azar by 2017 and Lymphatic Filariasis by 2017.
- To reduce the prevalence of blindness to 0.25/ 1000 by 2025 and disease burden by one third from current levels.
- To reduce mortality from cardiovascular diseases, cancer, diabetes or chronic respiratory diseases by 25% by 2025.
Health Systems Performance
Health Services
- Increase utilization of public health facilities by 50% from current levels by 2025.
- Antenatal care coverage to be sustained above 90% and skilled attendance at birth above 90% by 2025.
- More than 90% of the new born are fully immunized by one year of age by 2025.
- Meet need of family planning above 90% at national and sub national level by 2025.
- 80% of hypertensive and diabetic individuals at household level maintain "controlled disease status" by 2025.
Sectoral goals related to health
- Relative reduction in prevalence of current tobacco use by 15% by 2020 and 30% by 2025.
- Reduction of 40% in prevalence of stunting of under-five children by 2025.
- Access to safe water and sanitation to all by 2020 (Swachh Bharat Mission).
- Reduction of occupational injury by half from current levels of 334 per lakh agricultural workers by 2020.
- National/ State level tracking of selected health status.
Health Systems strengthening
Health finance
- Increase health expenditure by Government as a percentage of GDP from the existing 1.1 5 % to 2.5 % by 2025.
- Increase State sector health spending to > 8% of their budget by 2020.
- Decrease households facing catastrophic health expenditure by 2025 from the current levels by 25%.
Health Infrastructure and Human Resource
- Ensure availability of paramedics and doctors as per Indian Public Health Standard (IPHS) norm in high priority districts by 2020.
- Increase community health volunteers to population ratio as per IPHS norm, in high priority districts by 2025.
- Establish primary and secondary care facility as per IPHS norms in high priority districts by 2025.
Health Management
- Ensure district - level electronic database of information on health system by 2020.
- Strengthen the health surveillance system and establish registries for diseases of public health importance by 2020.
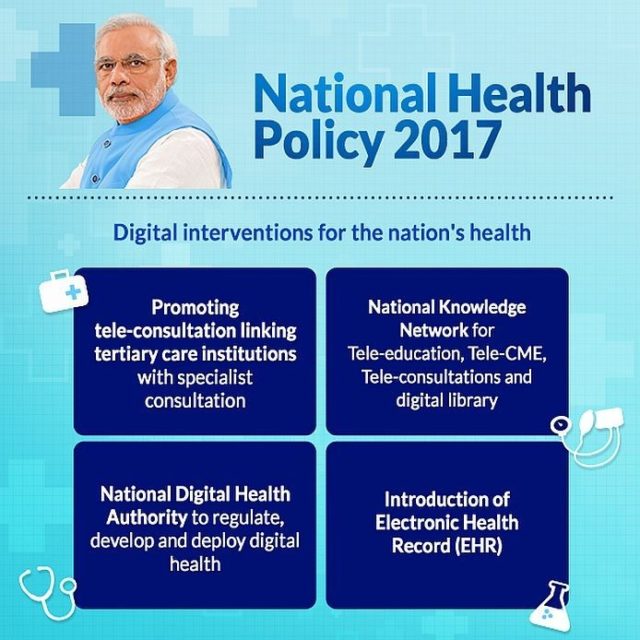
- Establish integrated health information architecture, Health Information Exchanges and National Health Information Network by 2025.
Policy thrust
- Ensuring Adequate Investment - The policy proposes a potentially achievable target of raising public health expenditure to 2.5% of the GDP in a time bound manner.
- Preventive and Promotive Health - The policy identifies coordinated action on seven priority areas for improving the environment for health:
- The Swachh Bharat Abhiyan
- Balanced, healthy diets and regular exercises.
- Addressing tobacco, alcohol and substance abuse
- Yatri Suraksha – preventing deaths due to rail and road traffic accidents
- Nirbhaya Nari – action against gender violence
- Reduced stress and improved safety in the work place
- Reducing indoor and outdoor air pollution
- Organization of Public Health Care Delivery - The policy proposes seven key policy shifts in organizing health care services.
--------------
Leave a Reply
Your Comment is awaiting moderation.


